Preliminary data from California on COVID-19 cases and deaths through May 20, 2020 suggest racial/ethnic disparities in adults diagnosed and dying from the disease caused by the novel coronavirus, SARS-CoV2. While there were substantial amounts of missing data (30% of cases and 2% of deaths were missing information on race/ethnicity) and data are dependent on testing to identify cases, two patterns have emerged. First, adults of Latino and Native Hawaiian/Pacific Islander race/ethnicity are disproportionately more likely to be infected with SARS-CoV2 relative to the proportion of the California population that they make up. Adults of African-American/Black race/ethnicity made up a greater proportion of deaths from COVID-19 relative to their proportion of the California population. The demographic data do not tell us why these patterns may exist but some hypotheses have been put forth. Cases, which indicate infection with COVID-19, may be associated with socioeconomic factors, such as, employment in essential occupations, being less able to work from home or less able or compliant with social distancing. Deaths, which indicate more severe disease once infected, may be reflective of less access to health services, more prevalent comorbidities, or vitamin D deficiency (vitamin D is essential to immune function). More research is needed to examine these potential racial/ethnic disparities.
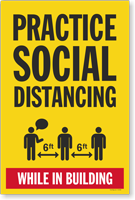
Tag: social distancing
Pandemic EpiSpeak
Students who have taken one of my classes in epidemiology at CGU will probably remember me saying that learning epidemiology is, in many ways, comparable to learning a new language. Like many other fields, in epidemiology, we use specific words to indicate specific things. Hopefully my students are having fond memories right about now of the terminology we learned in class, for example, to describe disease occurrence in populations.
Our “EpiSpeak” also includes terms used in efforts control epidemics, as we are currently with the COVID-19 pandemic. I’ve heard some mixing of terms circulating such as referring to our stay-at-home order as “quarantining”.
Here is some clarity on three key terms: isolation, quarantine and physical distancing (also called social distancing) citing the World Health Organization.
“Isolation means separating people who are ill with symptoms of COVID-19 and may be infectious to prevent the spread of the disease.”
“Quarantine means restricting activities or separating people who are not ill themselves but may have been exposed to COVID-19.” By anticipating who might become sick, the goal is to prevent spread of the disease at the time when people just develop symptoms.
“Physical distancing means being physically apart. WHO recommends keeping at least 1-metre (3 feet) distance from others. This is a general measure that everyone should take even if they are well with no known exposure to COVID-19.” A goal of physical distancing is to slow the spread of disease by reducing the number of interactions we have with each other.
Be a steward of epi and apply these terms precisely! A benefit of this, I hope, is that we can reduce some of the confusion that is circulating and help to answer the question, “what can I do in the face of this pandemic”?